Summary:
Defining Acute Pain: Your Body's Initial Alarm System
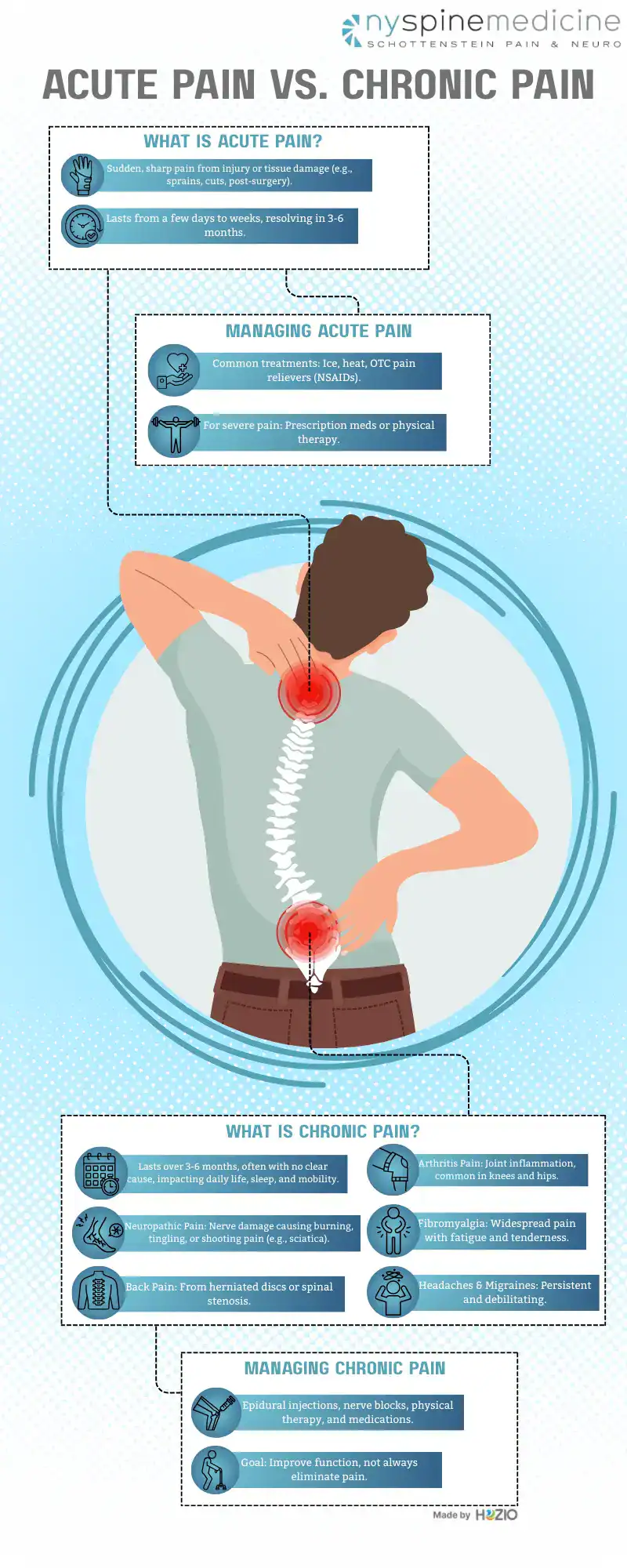
Acute pain is like your body’s immediate alarm system. It typically begins suddenly and has a clear, identifiable cause. Think about the sharp sting from a papercut, the throb of a sprained ankle after an awkward step on an uneven NYC street, or the soreness you feel after a dental procedure or surgery. This type of pain is a direct response to tissue damage or injury. Its duration is relatively short, usually lasting for a few days up to a few weeks, and generally resolves within three to six months as the underlying cause heals. The intensity of acute pain can range from mild to severe, but its primary role is protective, signaling you to stop, take notice, and address the injury to prevent further harm. If you’ve experienced sudden back pain after lifting something heavy, or neck pain from an abrupt movement, that’s typically acute pain sounding its warning.
How Acute Pain Typically Resolves and Its Management
In most instances, acute pain diminishes and disappears as your body’s natural healing processes repair the injured tissue. Treatment for acute pain primarily focuses on addressing the root cause—setting a broken bone, for instance—and providing pain relief to keep you comfortable during recovery. This might involve simple measures like applying ice to reduce swelling in a joint, using heat to relax muscle spasms, or taking over-the-counter pain relievers such as ibuprofen or naproxen, which are non-steroidal anti-inflammatory drugs (NSAIDs). For more intense acute pain, a pain specialist might prescribe stronger medications for a short period or suggest specific physical therapy exercises to restore movement and prevent stiffness.
When Acute Pain Signals a Deeper Concern
In most instances, acute pain diminishes and disappears as your body’s natural healing processes repair the injured tissue. Treatment for acute pain primarily focuses on addressing the root cause—setting a broken bone, for instance—and providing pain relief to keep you comfortable during recovery. This might involve simple measures like applying ice to reduce swelling in a joint, using heat to relax muscle spasms, or taking over-the-counter pain relievers such as ibuprofen or naproxen, which are non-steroidal anti-inflammatory drugs (NSAIDs). For more intense acute pain, a pain specialist might prescribe stronger medications for a short period or suggest specific physical therapy exercises to restore movement and prevent stiffness.
Want live answers?
Connect with a NY Spine Medicine expert for fast, friendly support.
Understanding Chronic Pain: A Persistent and Complex Challenge
Chronic pain presents a vastly different scenario. Unlike its acute counterpart, chronic pain persists for an extended period, typically defined as pain lasting longer than three to six months, or pain that continues even after the initial injury has seemingly healed. Sometimes, chronic pain can develop without any clear initial injury or cause, making conditions like fibromyalgia or some types of neuropathic pain particularly baffling for those who experience them. The critical aspect here is that the pain signals in your nervous system may keep firing for weeks, months, or even years. This ongoing discomfort can profoundly affect your daily life, often leading to reduced mobility, difficulty sleeping, fatigue, and even emotional distress such as anxiety or depression. For many NYC residents juggling work and personal life, chronic pain can reduce overall quality of life by a significant margin, sometimes by as much as 30-50% if not managed effectively. Addressing “what is the difference between acute and chronic pain, and why does this distinction matter for treatment?” becomes paramount when pain lingers.
Common Types and Sources of Chronic Pain You Might Experience
Chronic pain isn’t a single entity; it encompasses a wide range of conditions. You might be dealing with chronic back pain from a herniated disc or spinal stenosis, or persistent neck pain from degenerative disc disease. Arthritis pain, a common source of chronic joint pain, results from inflammation and wear and tear in joints like the knees or hips. Neuropathic pain arises from damage or dysfunction of the nerves themselves, leading to sensations like burning, tingling, or shooting pains; sciatica is a prime example. Conditions like fibromyalgia cause widespread musculoskeletal pain accompanied by fatigue and tenderness. Chronic headaches and migraines can also become a persistent burden, severely impacting daily routines. Each of these conditions requires a specialized approach to pain management.
Why the Distinction Between Acute and Chronic Pain is Vital for Your Treatment Plan
The reason “what is the difference between acute and chronic pain, and why does this distinction matter for treatment?” is so important is because the approaches to managing them are fundamentally different. Acute pain treatment aims to eliminate the pain by healing the injury, using methods like short-term medication, rest, or physical therapy to restore normal function quickly. However, for chronic pain, the goal often shifts from complete elimination to functional restoration and improved quality of life. A pain clinic or pain specialist in NYC will employ a multidisciplinary strategy. This may include interventional pain management techniques such as epidural steroid injections to reduce inflammation around spinal nerves, nerve blocks using local anesthetics like lidocaine to interrupt pain signals for conditions like joint pain, or radiofrequency ablation for longer-term relief from certain types of back pain or neck pain. Medications might include different classes, such as anticonvulsants for neuropathic pain, alongside physical therapy and lifestyle adjustments. A properly designed chronic pain management plan can significantly decrease reported pain levels, often by 3-4 points on a 10-point scale, and improve your ability to engage in daily activities by over 40%.
Taking Control of Your Pain Journey in NYC
In summary, recognizing “what is the difference between acute and chronic pain, and why does this distinction matter for treatment?” is the cornerstone of an effective pain management strategy. Acute pain acts as a temporary alarm, while chronic pain is a persistent condition that requires a more sustained and often multifaceted approach. If you are struggling with pain, whether it’s a recent injury causing acute back pain or a long-standing issue like arthritis pain or neuropathic pain that has become chronic, understanding its nature helps you seek the right care. Don’t let pain dictate your life in NYC. If discomfort lingers or significantly impacts your well-being, reach out to a qualified pain specialist. They can provide an accurate diagnosis and develop a personalized pain relief plan to help you regain control and improve your quality of life. Contact us today to learn how specialized interventional pain management can address your specific needs.






